January is Cervical Health Awareness Month
 It’s the new year. It's Cervical Health Awareness Month. It's time to get a Pap test.
It’s the new year. It's Cervical Health Awareness Month. It's time to get a Pap test.
Now get comfy, because this blog is going to go deep.
January 2020 is Cervical Health Awareness Month in the United States. Which makes this a great time for everyone to increase our awareness of cervical cancer and the screening methods.
According to the Canadian Cancer Society, an estimated 1350 Canadians were diagnosed with cervical cancer in the year 2019. Early detection of cervical cancer is key in identifying pre-cancerous changes in the cervix. The earlier you are diagnosed and treatment begins, the better the outcomes.
A Canadian has a better chance of responding to treatment and survival with early detection…
So let’s talk about your cervix, the cervical cancer screening tests and the impact on the pelvic floor!
WHAT IS YOUR CERVIX?
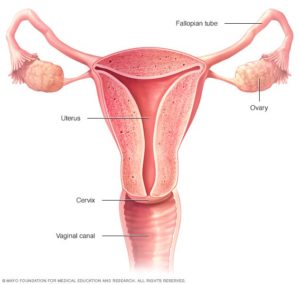 The cervix is the lowest part of the uterus. It opens up into the top of the vagina. You can think of it as the passageway that connects the uterus to the vagina.
The cervix is the lowest part of the uterus. It opens up into the top of the vagina. You can think of it as the passageway that connects the uterus to the vagina.
The cervix is very small, only measuring 2 to 3 cm long (1 inch) and generally cylindrical in shape. It is made up of fibromuscular tissue (muscle and connective tissue) and has two parts:
- Ectocervix: protrudes into the vagina
- Endocerix: opens up to the uterus
These two parts are made up of different types of cells, and the border between the parts is called the transformation zone. Precancerous cells are often identified in this zone.
WHY IS YOUR CERVIX IMPORTANT?
The cervix doesn’t just form the connection between the uterus and vagina. Although small, it is mighty!
It produces mucus that protects the uterus, ovaries and fallopian tubes from bacteria. The mucus also changes in consistency during the menstrual cycle and plays a role in the monthly sloughing of the endometrial cells.
The cervix also changes significantly during late pregnancy and birth. The cervix moves, thins (or ripens), and dilates during childbirth. This allows the baby to pass from the womb into the outside world! (For more information on how the cervix functions during pregnancy and childbirth, consider reserving a private prenatal class with on of our Certified Childbirth Educators.)
WHAT ARE COMMON PROBLEMS OF THE CERVIX?
Like all other cells in our body, cells in the cervix sometimes change and no longer grow normally.
These changes can lead to non-cancerous (benign) tumours such as polyps, cysts or fibroids; or grow to be precancerous conditions. “Precancerous” means that the abnormal cells are not yet cancer, but there is a chance that they may become cancer if they aren’t treated.
Here is a list of some common problems of the cervix:
- Cervical polyps: Small growth on the part of the cervix that connects to the vagina. Usually harmless and painless.
- Cervicitis: Inflammation of the cervix. The cause can be many things: a sexually transmitted infection (chlamydia, genital herpes, trichomoniasis, etc.) or bacterial infection. An allergic reaction to condoms or hygiene products can also cause a reaction. You may experience painful urination, unusual discharge from the vagina, bleeding and/or painful sex.
- Cervical incompetence: The cervix widens during pregnancy well before the baby is due, which can lead to premature delivery.
- Cervical cancer: Common signs and symptoms of cervical cancer include vaginal bleeding, abnormal discharge and dyspareunia. The process of diagnosis may be long and frustrating because other health conditions can cause similar symptoms. Usually, the diagnosis begins when a Pap test becomes abnormal and cells in the transformation zone of the cervix show precancerous changes including dysplasia and lesions.
There are some factors that may increase your risk of precancerous changes and cervical cancer. These risk factors may include: smoking, weakened immune system, Human Papillomavirus infection, and/or family history.
HOW SHOULD I PROTECT MYSELF?
There are many ways to screen for cervical conditions but the BEST way is through a Pap test by a physician. Pap tests help find conditions like cervical cancer BEFORE any symptoms develop.
The Canadian Cancer Society recommends getting a Pap test starting at the age of 21 if you have ever been sexually active. Pap tests should take place every one to three years, depending on the results of your last Pap test. Screening can stop after age 65 or if a hysterectomy has been performed (removing the cervix).
WHO SHOULD BE TESTED?
The answer is clear: anyone with a cervix.
Most of the current information focuses on cervical health for cisgender women (women whose gender identity align with their biological sex assigned at birth). However, the risk of cervical conditions including cervical cancer affects transgender assigned female at birth (AFAB) individuals who have a cervix.
It is important to note that some patients who are transgender face barriers in receiving medical treatment including discrimination and lack of culturally competent and sensitive health care providers. This may lead them to defer internal vaginal examinations including a Pap test, thereby presenting late detection of any pre-cancerous or cancerous changes.
There are resources in Toronto to help AFAB individuals find healthcare providers who are trans-friendly and knowledgeable. Rainbow Health Ontario is a great place to start!
HOW DOES CERVICAL HEALTH IMPACT THE PELVIC FLOOR?
Pelvic floor muscles support organs including the uterus and cervix. When you and your organs are experiencing symptoms of pain or not working in a healthy manner, the pelvic floor muscles can often tighten up.
Tight, shortened pelvic floor muscles are not happy. They are often painful to the touch, pressure and/or movement. Unhappy pelvic floor muscles can negatively impact how we perform activities of daily living including toileting practice and sexual function. Many individuals find their pelvic floor is impacted by pregnancy and birth.
Additionally, treatment for cervical cancer such as hysterectomy can lead to tight pelvic floor muscles leading to pelvic pain and bladder/bowel concerns. Scar tissues from surgery can also lead to persistent pelvic pain.
A pelvic health physiotherapist can help to relieve pelvic pain with scar management, tender point releases and other techniques that are supported by research. Education can be provided relating to your condition and the effect on your bladder and bowel. A pelvic health physiotherapist can collaborate with your entire medical team to ensure that you are at the centre of a comprehensive care plan.
Have more questions? Book an initial meeting with Michiko Caringal, Pelvic Health Physiotherapist!
Contact information:
Michiko Caringal, MScPT, MHSc in Bioethics
Website: www.happydownthere.ca
Tel: 416-892-1156
Email: michiko@happydownthere.ca
IG: @happydownthere
